A 31 years old male patient presented in the emergency with mild slurring of speech and chest discomfort for 3 days. On examination, he had BP - 240/130 mmHg, PR – 84/min, chest - bilateral vesicular breath sounds, no pedal edema. He presented with hypertensive emergency and was managed in the emergency with inj Lasix and inj labetalol. Further evaluation revealed USG abdomen – left kidney measures 11.5*5.7 cm, right kidney- non-functional, calcified right renal parenchyma. USG renal doppler suggestive of right renal artery narrow in calibre, likely chronic thrombosis. ECG- LVH strain pattern. MRI brain revealed acute lacunar infarct in posterior limb of left internal capsule. The patient has been diagnosed with renovascular hypertension, unilateral renal artery stenosis (? Takayasu arteritis) and acute ischemic stroke. He has been managed conservatively with anti-hypertensives and antiplatelets.
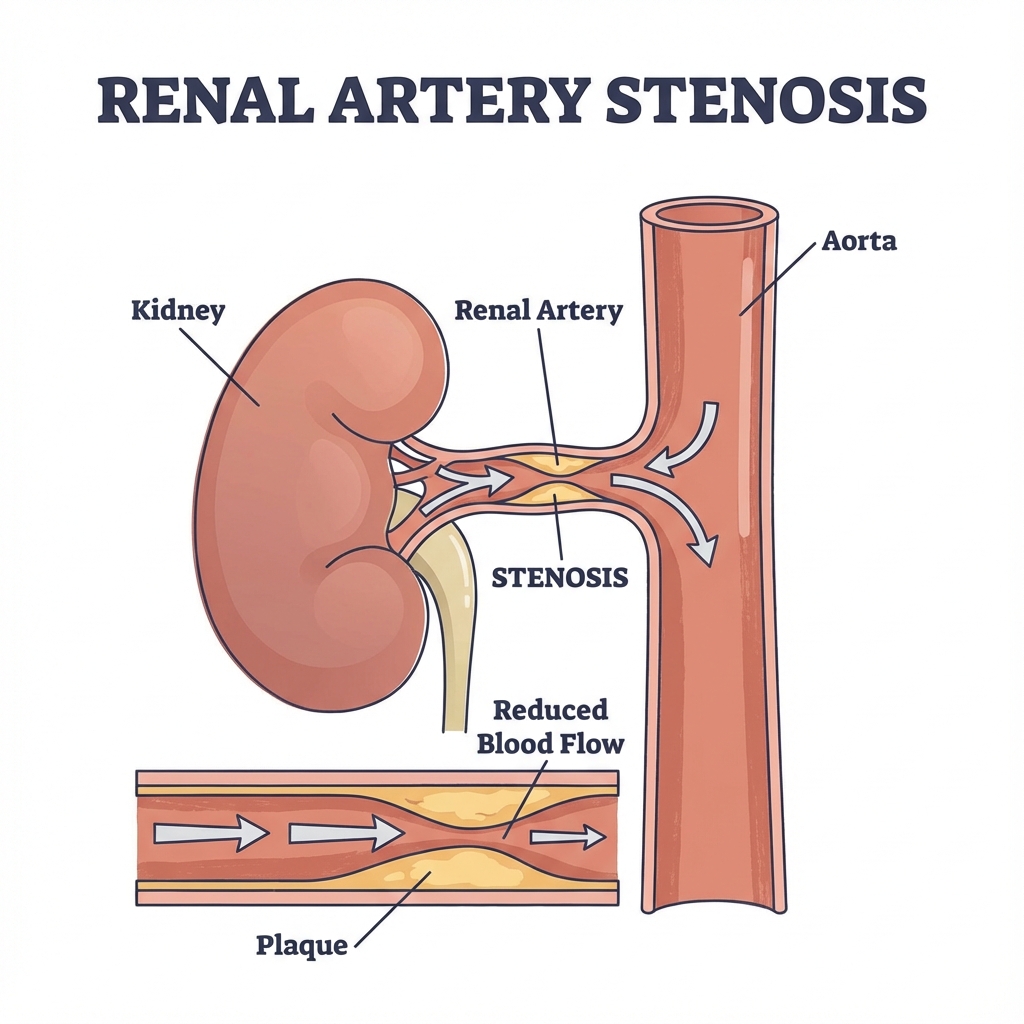
Renal Artery Stenosis Diagram
Renovascular Hypertension
Definition: Renovascular disease is an important, potentially correctable cause of secondary hypertension. Renovascular hypertension is a clinical syndrome marked by a rise in arterial pressure and associated with reduced perfusion in the kidneys with or without associated ischemic and hypertensive renal injury.
Epidemiology: The most common cause is renal artery stenosis. It accounts for around 5% of all hypertensives.
Etiopathogenesis
Atherosclerosis (70 %, mostly bilateral), fibromuscular dysplasia (30%), Takayasu arteritis.
Pathophysiology
Two-Kidney, One-Clip Model
Hypertension dependent on ANGIOTENSIN-II-induced vasoconstriction. Managed with reversal of the RAS, with ACE inhibition, or with angiotensin receptor blockade.
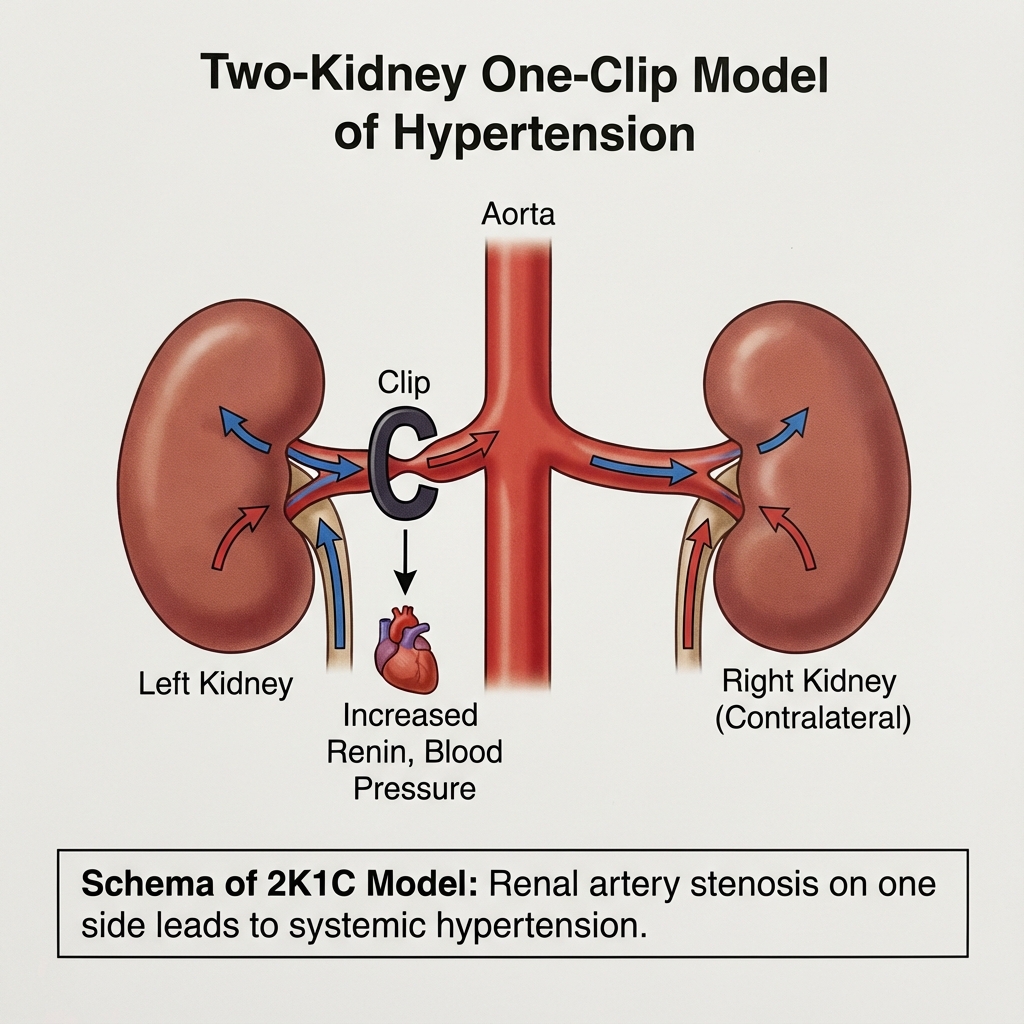
Two-Kidney One-Clip Model
One-Kidney, One-Clip Model
Hypertension in the one-kidney, one-clip model is largely maintained by volume and sodium excess in the presence of normal circulating A-II levels. Plasma renin levels normal. Diuretics are helpful.
Management
Goals of treatment:
- Control hypertension
- Prevent deterioration in renal function
Management protocols depend on whether unilateral or bilateral disease, type of disease, degree of ischemic nephropathy, level of blood pressure and lipid profile.
Long-term management of these patients require integrated pharmacologic management of blood pressure and cardiovascular risk combined with optimal management of lipid profile and lifestyle modifications (diminishing tobacco use).
ACEi/ARBs are effective in patients with renovascular disease, diuretics, anti-platelets, statins and management of hyperglycemia are often needed.
Revascularisation options include: percutaneous angioplasty with stenting or surgical revascularisation in patients with complex anatomic lesions. They are indicated only in the following conditions:
- Failure of optimal medical therapy to control blood pressure
- Intolerance to optimal medical therapy
- Recurrent flash pulmonary edema and/or refractory heart failure
Large trials like CORAL (n=947), ASTRAL (n=806), STAR trials have concluded that revascularization carried substantial risk but was not associated with any benefit with respect to renal function, blood pressure, renal or cardiovascular events, or mortality when compared in a randomized large trial with medical therapy alone. The principles and success of vascular intervention in the coronary and peripheral arteries may not extend to the renal circulation likely because kidneys receive an excess of oxygenated blood, far more than needed for basal metabolic demands.
Conclusion
To conclude, renovascular hypertension is not an uncommon finding and clinicians need to have a high suspicion of this condition in order to prevent long term cardiac and renal morbidity.